Red eyes usually come in pairs and so do podcasts on the subject. In part two of the red eye disorders we discuss the non-threatening maladies that can turn into eye threatening disorders if missed. Sit back and relax and let dear ole' dad tell you one more time why it's going to be OK...If you listen to him. Otherwise you may get spanked. I'm serious he spanked me a lot for not listening. Call CPS; there's still a chance for me....
The Eyes Have It..... Or At Least The Red Eyes Do
Harold Andrew Sloas Jr, DO, CAPT, USN-R is a board certified ophthalmologist (and my dad). He had a competition with his son Harold Andrew Sloas III, DO, RDMS, FAAEM to see who could get get more letters behind their name. As it turns out none of those letters have any bearing on what we'll be talking about today.
You're in for a real treat because I got to sit down with dear ole' dad and talk about some red eye disorders. We explore all the threatening causes of the red eye on this podcast and move into the non-threatening red eye disorders on the next episode. You need to know something about both so you can distinguish between the two. Pull out your Kleenex and dry your eyes; you're going to need to see this.
Pediatric Concussion
I have had the opportunity to work with some truly amazing people in my life and Dr. Matt Bayes, sports medicine physician extraordinaire, is no exception. Dr. Bayes is the only person I have known to successfully ask about a “code red” and somehow avoid receiving one. Dr. Bayes now resides in St. Louis, Missouri (Bayes from The Lou) and has been part of the sports medicine team that delivers care to the St Louis Cardinals. On this episode Dr. Bayes takes me through the intricacies of diagnosing and managing a pediatric concussion from the ER perspective. Hold on to your head because you’re about to get knocked out....Smokey
ARTICLES:
William R. Mower, MD. What Rules Should Guide Imaging Decisions in Injured Children? Medscape. Posted: 02/23/2010. http://www.medscape.com/viewarticle/717110
Evaluating Minor Head Injury - Sports Medicine Update
Pediatrics - Sports Related Concussions and Management
Pediatrics - Emergency Department Visits for Concussion in Young Athletes
Misconceptions Common With Pediatric Concussions
José Álvarez-Sabín, MD; Antoni Turon; Manuel Lozano-Sánchez; José Vázquez, MD; Agustí Codina, MD Delayed Posttraumatic Hemorrhage "Spät-Apoplexie"Stroke. 1995;26:1531-1535doi: 10.1161/01.STR.26.9.1531
Dr Matt Bayes Contact Info:
12855 North Forty Drive
Suite 380
St Louis, MO 63141
Ph: 314-434-7784
Fax: 314-434-4775
www.bluetailmedicalgroup.com
Calcium Channel Blockers, Beta Blockers and Undifferentiated Hypotension....OH MY!
One of the most sphincter tightening overdoses to deal with in adults and pediatrics is the CCB overdose. In this podcast I cover all the treatments that work, don't work, and you would think should work to give you a recipe for success. Hold on to your insulin; it's not just for diabetics and critically ill patients anymore. Intralipids??? How the heck does that help??? Well you need to tune in to find out......
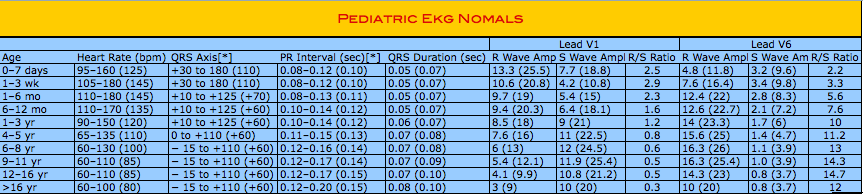
Pediatric ECG Basics ~ Part 2
Our resident cardiologist Dr. Buck Kyle completes the second part of his lecture series on pediatric ECG reading. This time we get into the most common cardiac disease processes that occur in the pediatric population. What’s black and white and read all over??? OK, yes the newspaper, but ECGs are too....don’t steal my punch lines.....
Pediatric (and some adult) ECG Basics
The Squiggly Line Rule: The more squiggly lines in the outline/border lines of a state, the cooler/more fun it is to live in that state. In, for example, the state of California, the squiggly lines are found on the coastline adjacent to the pacific ocean ~ Urban Dictionary
It also happens to be true that if you are an electrocardiogramophile than the more abundant the squigglies, the more stimulating and salacious the ECG is to read (and you probably have eroticism issues). While it is also true that if you do not find electrocardiogram interruption to be lascivious than you probably find it to be frustrating (and you may have ECG performance issues). Either way, have I got a tonic for you. It cures all of the above (except the obvious sexual innuendo problems, you need to see a therapist for that soon).
In this episode, we start a two part series on the basics of pediatric ECG interruption with Dr. Buck Kyle, pediatric cardiologist and electrocardiogram aficionado. Sit back and relax as Dr. Kyle makes everything clear and really...see the therapist soon......
Penis Talk ~ With Your Hosts Sloas and Stroup
The finale in the Urology trilogy. In this episode Dr. Sean Stroup, CDR, USN, MC and I wrap-it-up with a series of "down-there" complaints (down-there does not imply that this episode is about Australians with grievances) with the most sensitive of subjects to any male patient, penile complaints, worries about the willie, persevering about the pee pee, jargon about the junk, etc. Hold on to your hats....
The Disclaimer hasn't changed: if you think jokes about "shrinkage" are funny than please listen to the podcast, but if you find those offensive then skip this episode and I wish you all the best in your attempt to make it through your career without encountering another penis...again....ever.
Urology Part 2 ~ The Painless Scroti
"Amigo, the only thing in this world that gives orders is balls. Balls. You got that?" ~ Scarface 1983
Every man is attached to their nuts. In this episode CDR Sean Stroup, MD USN and I continue to discuss non painful ballular complaints. You make think your safe with a non-painful swollen scrotum, but oh contraire mon frere, you can lose a nut that way too. A guy just can't get a break....
The Disclaimer from the last episode still applies: if you think jokes about old man balls are funny then please proceed to listen to this podcast, but if you find those offensive then skip this episode and look into non-urologic career paths. However, if you do listen to this podcast then the ball you save could be your own....
Urological Complaints Part 1 - The Painful Scrotum
"Rub your balls, squeeze your balls so you don't get cancer" ~ Tom Green
Few things cause more pain for the patient and fear in the practitioner than scrotal discomfort in a child. I sat down with my good friend and pee-pee doctor CDR Sean Stroup, MD USN at the National Naval Medical Center in sunny, beautiful, oh how I miss it: San Diego, to discuss painful ballular complaints. Dr. Stroup is a fellowship trained urologist practicing on the west coast and sees a ton of children at the Naval Medical Center. Disclaimer: If you are offended by jokes about pee-pee, the scroti, or not wearing appropriate underwear than it is probably best to skip this episode. No testicles were injured or neutered in the production of this podcast.
Podcast 10 - Urological Complaints Part 1: The Painful Scrotum
Ketofol & Shah
I had the privilege to sit down with one of Canada’s finest, Dr. Amit Shah, and discuss his blinded randomized prospective study concerning one of my favorite procedural medications: Ketofol.
This is the evidence based follow-up to my last (more opinion based) podcast on “Sedation and Ketofol.” The chocolate in my peanut butter.......
Shah A, Mosdossy G, McLeod S, Lehnhar, Peddle M, Rieder M. A blinded randomized controlled trial to evaluate ketamine/propofol versus ketamine alone for procedural sedation in children. Ann Emerg Med. 2011 May;57(5):425 33.e2. Epub 2010 Oct 13. PubMedPMID: 20947210
Sedation and Ketofol
There are a lot of ways to sedate, but I would like to provide you with a philosophy and the methodology to put together the safest possible sedation package.
Please stay tuned for my next episode in which I get a chance to interview Dr. Amit Shah the lead author on the game-changing Ketofol article listed below.
Shah A, Mosdossy G, McLeod S, Lehnhardt K, Peddle M, Rieder M. A blinded,randomized controlled trial to evaluate ketamine/propofol versus ketamine alonefor procedural sedation in children. Ann Emerg Med. 2011 May;57(5):425-33.e2.Epub 2010 Oct 13. PubMed PMID: 20947210
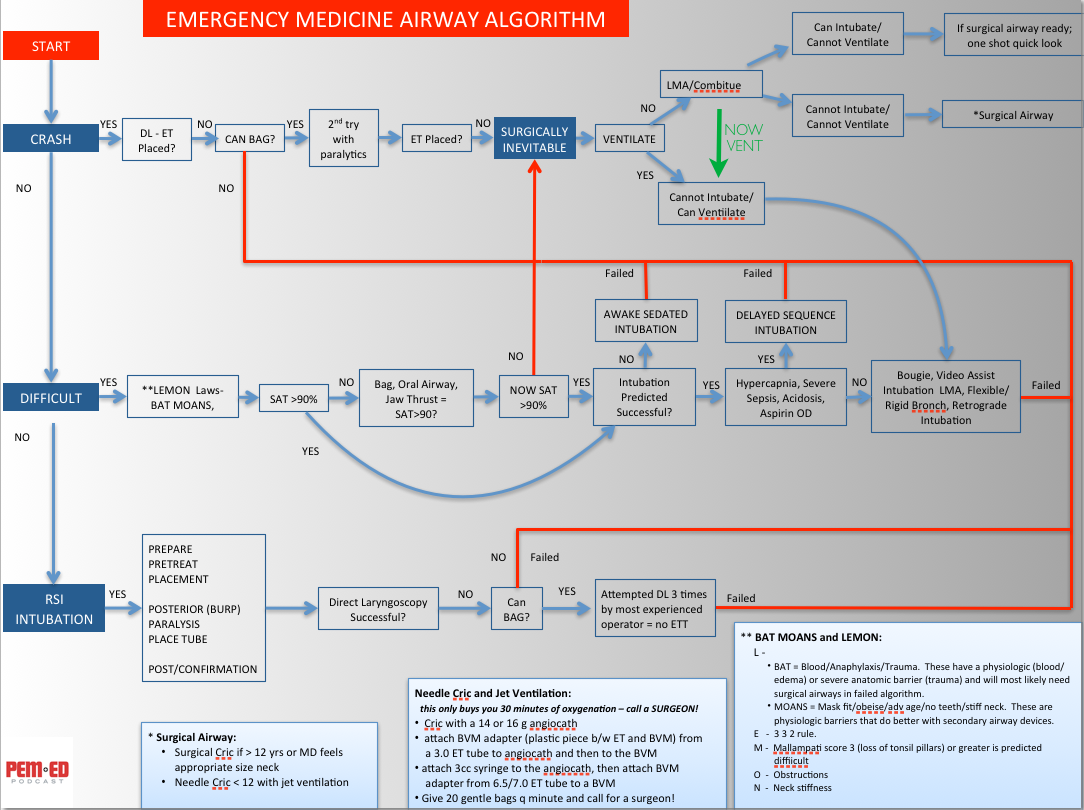
Pediatric Airway - The Advanced Course
This is the second part of a two part series in pediatric airway management. Here we focus on how to use the "Airway Algorithm" that we have created and how to manage the more difficult airways we encounter in the emergency department. The "Airway Algorithm" is designed to be used in both adults and children.
Reference: The Difficult Airway Course: Emergency™ (http://www.theairwaysite.com) and from Walls RM and Murphy MF: Manual of Emergency Airway Management, 4th Edition, Philadelphia, Lippincott, Williams and Wilkins, 2012.
Pediatric Airway 101
“Airway is the reason that many go into emergency medicine…”
- Jaime McCarthy MD, UT Health Sciences Center at Houston EM Director
One of the many things that we do better than anyone in the business is obtain the emergent airway. Unlike our colleagues in other disciplines, we do not have the luxury of planning our airway approach on the golf course the evening before; we meet patients on their worst day. Even though we would often prefer it, we do not have the option to reschedule our intubations.
Smashed, bloody, distorted, edematous, airways secondary to trauma, anaphylaxis and GI bleeds are the things that we deal with routinely with nary a complaint or even a hither for a better look than what were given. We often feel lucky to get any type of view that resembles normal laryngeal anatomy. Personally, if I knew that I would need to be intubated today, that my airway would be bloody and edematous, and there was only time for one person to take a shot at placing the tube, then I would pray to God that the last face I see before the Roc and Etomidate push me asunder is the familiar grill of one of my EM colleagues. Who better to bet all my chips on then someone who deals with the hardest airways on the face of the planet as part of their daily routine? The general EM provider can not only get that airway, but is so relaxed about it that they will casually check on the patient in the next bed before and after the intubation. That’s the confidence I’m looking for when it comes to the fast paced life and death world of emergency airway.
Whether it is pediatric or adult emergency medicine, the most important thing that we do as “emergentologists and resusitologists” is control the airway.
Clearing The Pediatric C-spine
Developing a good rule to clinically clear the pediatric cervical spine would be difficult. Very few kids suffer injuries to that region of the body making it nearly impossible to create a well-powered decision instrument. Like with many other attempts in pediatrics you would most likely end up with a guideline that would be fairly sensitive, but horribly specific.
Lets say we abstracted and validated a pediatric c-spine rule that was 95% sensitive and 50% specific. With a disease that occurs at an incidence of less than 0.1% (1/1000), by employing a decision instrument that is 95% sensitive you would reduce your patient's risk of missed injury to say 0.005% (1/20,000) . Sounds great right? Hold on though; there's more. If that same rule is 50% specific (which most peds clinical rules are) 50% of the kids you applied your rule to will have false positives. Therefore 500 of every 1000 patients you employ your decision instrument for would actually be subjected to further workup and needless radiation.
Does any of that sound familiar? It's nearly identical to the use of D-Dimer in very low risk adults (probably better stated as no risk). If you take a low to medium pre-test probability of disease (Wells Score of low-mod = 2-16% risk) and apply a D dimer (sensitivity > 95%) that comes back as a negative result (you now have reduced your 16% chance of having disease to less than 1% because 16% reduced 95% is 0.8%). Well done! You are done with the work-up and you have excluded disease. If you apply the D-Dimer to a very low risk population (1-1000 to 1/10,000 depending on who you read) then you may further reduce your risk (I'm not sure how much lower you need to go to fell comfortable 1/1000 is pretty low), but just like in the example above, you will have subjected twice as many patients to needless CTA of their chests because your D-Dimer specificity was so poor (about the same 50% as above).
Sorry, that's a lot of stats, but here's the take-home message. Your pediatric patient doesn't need a decision instrument as much as they need a good doctor. Any injury with extremely low prevelence will most likely end up below the test threshold of creating and validating a decision instrument that you can rely on. It is hard to get objective data in pre-verbal children, but it is easy to play with them, earn their trust and make a good clinical decision. NEXUS gets you to 8 years of age, but then it's up to you to make a decision based on experience.
Podcast 5 - AVI Format (Larger Video Version)
An Easy LP Technique
If you downloaded the fist version of this (no intro music), delete it and re-downlad. The audio is much better on the second version.
Practitioners have a love-hate relationship with this procedure. Whether you embrace it or react to its’ necessity in the same manner you would when finding out you've just been cut-out out of your wealthiest relative’s will, the words “lumbar puncture” invoke emotion. I would like to thank Dr. David Delemos for inventing this simple recipe for success. It is one of my favorite procedures and hopefully after hearing this podcast it will be one of yours as well.
Check out the PDA friendly companion file below.
Fever of Unknown Source - Part 2
In this episode we complete our discussion on “Fever Without a Source” in the 2-3 month old population and also cover the 3-month plus age group. Again Dr. Andrea Cruz a subspecialist in emergency medicine and infectious disease at The Texas Children’s Hospital gives us some further insight into when and how to work these kids up.
Full disclosure: The author on two of the articles below is LCDR Sherry Rudinsky who is an old navy friend of mine. We were interns together and then attended the same Naval Flight School class. Dr. Carstairs is also an aquantaince; she was a resident when I was a Navy Surgical Intern. I was stationed at the Naval Medical Center San Diego when they were collecting their data, but I had no part in this study. They are simply dang good reads so check them out.
Fever Algorithm
References:
Reardon JM, Carstairs KL, Rudinsky SL, Simon LV, Riffenburgh RH, Tanen DA. Urinalysis is not reliable to detect a urinary tract infection in febrile infants presenting to the ED. Am J Emerg Med. 2009 Oct;27(8):930-2. PubMed PMID: 19857409.
Rudinsky SL, Carstairs KL, Reardon JM, Simon LV, Riffenburgh RH, Tanen DA. Serious bacterial infections in febrile infants in the post-pneumococcal conjugate vaccine era. Acad Emerg Med. 2009 Jul;16(7):585-90. Epub 2009 Jun 15. PubMed PMID: 19538500.\
Carstairs KL, Tanen DA, Johnson AS, Kailes SB, Riffenburgh RH. Pneumococcal bacteremia in febrile infants presenting to the emergency department before and after the introduction of the heptavalent pneumococcal vaccine. Ann Emerg Med. 2007 Jun;49(6):772-7. Epub 2007 Mar 6. PubMed PMID: 17337092.
Fever of Unknown Source - Part 1
Just in time for the winter season.....
Have you seen a bunch of snot-nose kids with fever recently? Do you want to put a needle in their back? Better yet, do you not want to put a needle in their back, but feel really guilty about it?
I sat down with Texas Children’s very own Dr. Andrea Cruz who is triple boarded in pediatrics, pediatric emergency medicine and pediatric infectious disease to talk about fever without a source in neonates/infants and who really needs that LP.
There are so many pearls here that I am going to break this into 2 podcasts. Enjoy part one now and don’t forget to check out the link to my “fever without a source” algorithm link below.
Undifferentiated Hypotension and the Modified RUSH Exam
This is my simplistic take on hypotension (ie. shock) in pediatric patients. All you need is an ultrasound, fluids and a basic understanding of the physiology.
Undifferentiated Hypotension Slide
Introductions are in order....
Welcome to PEM ED Podcast. Pediatric Emergency Medicine; an Educational and Directional Podcast for the general emergency medicine provider. I hope you find this podcast informative and practice changing. Please click on the link below and enjoy.